Shock experience and PTSD
Not every experience of a shock-event leads to a PTSD, in fact in many instances no PTSD will develop after such experience. So what are the factors which lead to a PDSD?
The emergence of a PTSD depends on the processing and landing of the of survival energies / survival instincts, which are being mobilised to deal with the event:
- If bodily survival energies are not used or discharged in safety after the shock event, they may get stuck in the body and lead to PTSD.
- If however the shock can be landed through safe social contact, a good understanding what happened and release of the survival energies, the person may be able to integrate the trauma and get on with life.
More information about the therapeutic work you find under Resolving Post Traumatic Stress (PTSD) through Body Psychotherapy.
Not every Shock event leads to PTSD. It depends how the person can land after the experience.
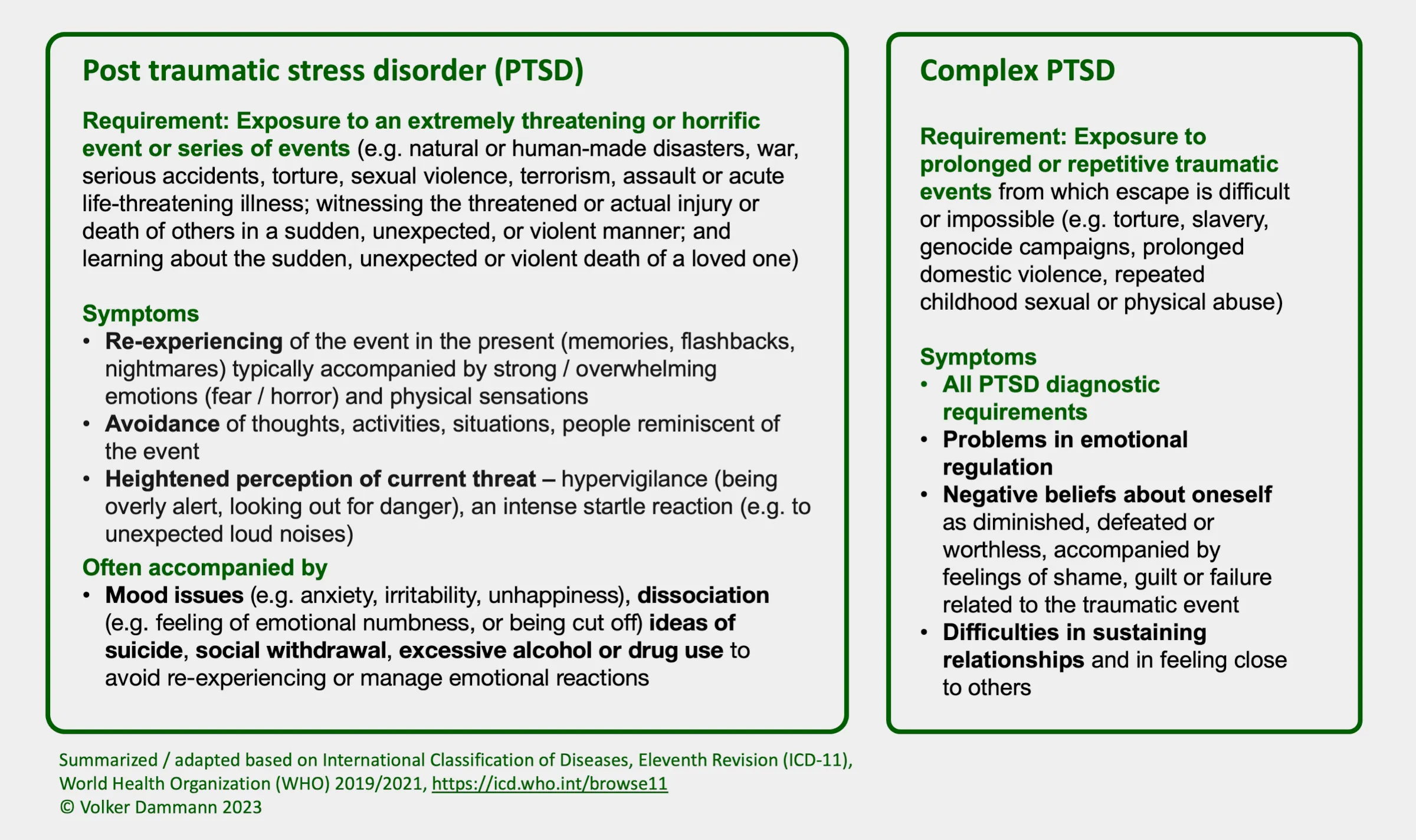
PTSD – Symptoms and Differential Diagnosis
Symptoms of post-traumatic stress disorder (PTSD) can significantly affect the quality of your daily life and your ability to function professionally and in social relationships.
PTSD Symptoms can include re-experiencing the event through intrusive thoughts, e.g. memories of the traumatic event, nightmares or flashbacks accompanied by a strong emotional reaction. Affected people may suffer from mood swings or emotional numbness. In addition they may also suffer from hyper-arousal, i.e. feeling irritable, on edge, and have difficulty sleeping or concentrating. In response, many sufferers avoid the triggers of these memories and therefore often withdraw socially. These symptoms can significantly impact daily life and relationships, and may last for months or even years after the traumatic event.
Specific Symptoms of PTSD
Specific Symptoms of PTSD include the following – compare international diagnostic criteria for PTSD as mentioned in ICD-10, diagnostic code F43.1 and ICD-11, diagnostic code 6B40:
- Re-experiencing – Re-experiencing the event through vivid intrusive memories, flashbacks, or repeated nightmares about the traumatic event
- Multiple sensory modalities possible: Re-experiencing may involving one or multiple sensory modalities (internal images, internal sounds or feelings).
- Overwhelming emotions: Re-experiencing is typically accompanied by strong or overwhelming emotions (particularly fear, horror and panic), and strong physical sensations (e.g. sweating, rapid heartbeat etc.).
- Trigger: Re-experiencing can be triggered by situations and circumstances, which are similar to the original shock-event.
- Hyper-arousal – Overall over-activation of the nervous system.
- Suffering from difficulties to fall asleep or be unable to sleep through the night.
- Irritability and being prone to anger outbursts.
- Strong startle reaction to stimuli reminding of the shock situation, such as unexpected noises, certain colors or smells
- Hyper-vigilance – Exaggerated watching out for potential threats
- Persistent anxiety and increased vigilance with regard to possible dangers / threats.
- Constantly watching out for possible danger or difficulties – even in situations which appear normally safe
- Avoidance of triggers and general withdrawal
- The person may avoid such situations, circumstances or people reminding of the event.
- The person may socially withdraw and may become difficult to reach for loved ones and suffer
- Depressive symptoms / Emotional numbness
- Mood swings or feelings of hopelessness
- An ongoing feeling of emotional numbness and blunting
- An inability to feel pleasure in normally pleasurable situations
- Thinking of suicide.
- Dissociation
- A feeling of detachment from other people and situations, unresponsiveness to surroundings (e.g. “everything feels muted or like behind a screen”)
Differential Diagnosis – Acute Stress Response
A PTSD is different from the an acute stress response:
- The acute stress response is part of the crisis, which develops as a direct reaction to the event. The acute stress response typically starts receding within 48 hours after the event and within a month, there is usually a marked decrease in symptoms of the acute stress response.
- In contrast, a PTSD may develop only a few weeks to a few months after the event, usually within 6 months after the event. A PTSD will only develop, if the traumatic event cannot be integrated appropriately in the post-shock crisis period through good support.
Differential Diagnosis – Complex PTSD
Complex PTSD (C-PTSD) is a relatively new term. It was officially introduced only in 2022 with diagnostic code 6B41 in the ICD-11, which came into effect only in 2022. The term C-PTSD is used to describe a set of symptoms that are more complex and severe than PTSD. C-PTSD is typically caused by prolonged and repeated traumatic experiences, such as childhood abuse or neglect, domestic violence, or ongoing exposure to violence or oppression.
A diagnosis of a C-PTSD requires that the criteria of a PTSD are met. In addition there are the following severe and persistent symptoms which cause difficulties in important areas of life (personally, with family, in school or workplace):
- problems with emotional regulation
- emotions of shame, guilt or failure related to the event
- negative believes about oneself (e.g. seeing oneself as worthless or defeated)
- difficulties in relationships
Complementary Treatment Approaches for PTSD
PTSD and C-PTSD can be treated with a combination of psychotherapy and – if necessary – medication. This typically involves trauma-focused cognitive behavioural therapy.
Newer or alternative psychotherapeutic approaches often involve the body, including approaches such as Somatic Experiencing®, Bodynamic® and Eye Movement Desensitization and Reprocessing (EMDR®). These methods can be used complementarily or within the framework of trauma-focused cognitive behavioural therapy.





